Most people who have periods can agree: They aren’t exactly fun.
Research has shown that heavy, painful and otherwise disruptive periods also can have a significant impact on someone’s life, such as missing more days of work.
The good news? If you have a uterus, you don’t need to have a period. There are safe, effective ways to stop getting a period for a little while or a long time. Here’s what you need to know.
What is menstrual suppression?
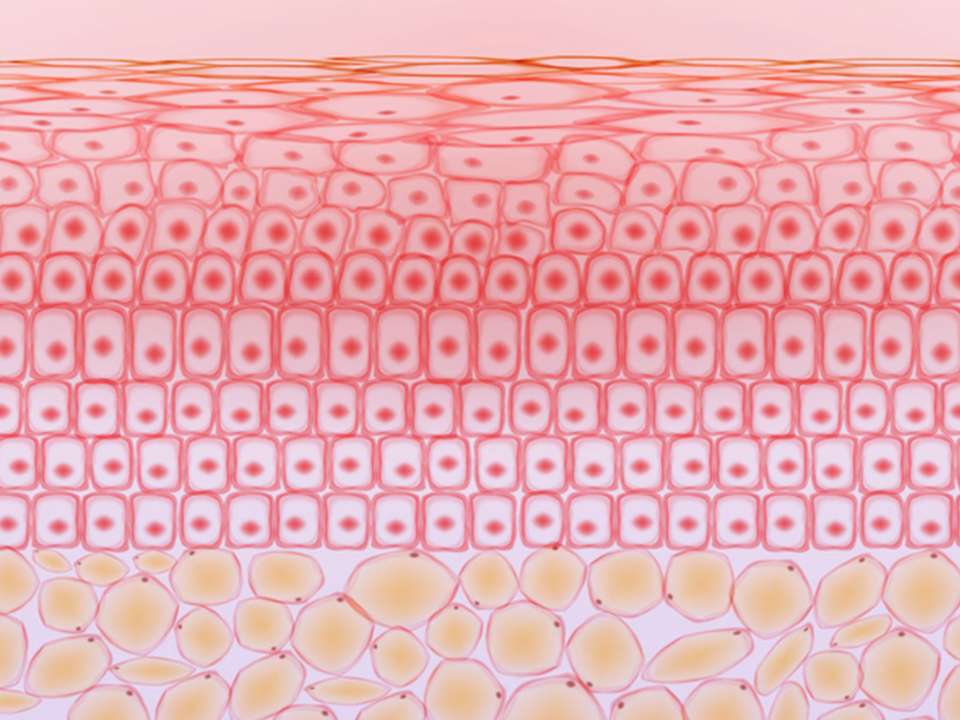
A refresher biology lesson: People who have a uterus, vagina and ovaries, and are between puberty and menopause, bleed around once every month. This involves thickening of the uterine lining, called the endometrium, which helps prepare the uterus for potential pregnancy.
It is entirely possible to stop this monthly bleeding by using hormonal birth control. Almost any hormonal method may stop someone’s period incidentally, whether or not the person actively tries.
“Not having a period can significantly improve someone’s quality of life and ability to interact in the world, plus fewer missed days at school or work,” Dr. Sarah Prager says. She is an OB-GYN at UW Medicine who specializes in family planning, birth control management, abortion and reproductive justice.
That is true for people who simply don’t want to deal with irritating monthly symptoms and for those whose periods prevent them from living a full life.
Being period-free is helpful for people who have a condition called menorrhagia, where they bleed so heavily they can develop anemia and, in rare cases, may need blood transfusions. It can also be helpful for people who have conditions such as endometriosis or polycystic ovary syndrome (PCOS), where periods may cause heavy bleeding and severe pain.
Some transgender and gender nonbinary people may not want a period because it causes dysphoria and doesn’t match their gender identity. Athletes, military personnel, or people who are outdoors or travel a lot for work may decide a period is an unnecessary hassle.
What birth control works best to suppress my period?
While many types of hormonal birth control could theoretically be used for menstrual suppression, some are more common or reliable than others. Birth control pills and IUDs are some of the most common methods, whereas IUDs and birth control shots are some of the most reliable.
There are several types of birth control pills: combination pills, which include both estrogen and progestin, and progestin-only pills. Among combination pills there are also monophasic and multiphasic. Monophasic means the amount of hormones in each pill is the same, whereas with multiphasic pills, the dose changes throughout the month.
Combination, monophasic pills are the easiest and most effective to use to stop your period. Most pill packets contain three weeks of active pills that have hormones and one week of inactive pills that don’t contain hormones. This is designed to mimic someone’s natural menstrual cycle. If you want to stop your period, you simply don’t take the inactive pills and instead go straight to the next set of pills that contain hormones.
Some brands, such as Amethyst, are designed to let you skip your period for a year or more. Others, such as Seasonique, are designed to give you a period only every three months.
Additionally, the contraceptive vaginal ring and transdermal contraceptive patches can both be used to reduce or eliminate periods with about the same effectiveness as pills.
The Depo-Provera birth control shot and high-dose IUDs are some of the most effective period-suppressing methods Prager prescribes for patients.
Hormonal IUDs such as Mirena and Liletta are the best option if you want an IUD and want to reduce or stop your period. (Copper IUDs, which don’t contain hormones, won’t work and may even make you bleed more heavily at first.)
Other methods, such as the arm implant, may stop periods in some people. If you want to try this method instead, it’s worth having a conversation with your doctor.
Is it safe to stop my period?
“There isn’t really anyone who couldn’t safely have menstrual suppression,” Prager says.
Naturally not having a period can sometimes be an indicator of a health issue — such as in people who have eating disorders, for example — but if you intentionally and safely stop your period, it isn’t risky, Prager says.
Prager’s logic is this: 200 years ago, for example, women tended to have more children and so spent much more of their life pregnant or breastfeeding (and not getting their period).
“Modern people with uteruses have many more periods than people did then,” she explains.
In some cases, using an IUD, shot or other form of birth control may be safer for someone than using birth control pills. While rare, birth control pills can increase stroke risk in some people who smoke and are over age 35, have high blood pressure, get migraines with aura, or have a history of stroke or heart disease.
While menstrual suppression isn’t dangerous, initiating hormonal birth control can be uncomfortable at first, depending on how your body reacts to the type of birth control you’re using. Some people experience mood changes like anxiety and depression, nausea, breast tenderness, migraines, weight fluctuations or other unpleasant symptoms.
For many people, these symptoms will go away within a few months. But some people may need to try a different form of birth control if their symptoms are too bothersome.
On the plus side, there are also benefits to taking birth control and stopping your period, Prager says.
Along with not having to deal with whatever unpleasantness bleeding brings, no period means no money spent on tampons and pads. It can also improve someone’s sex life, reduce the amount of sick days they take off from work, improve acne and reduce someone’s risk for endometrial (uterine) and ovarian cancer, Prager says.
If you already have acne, migraines, anxiety or depression, some kinds of birth control may make these things better.
How common is breakthrough bleeding?
If you’ve done any research on menstrual suppression, chances are you’ve heard of breakthrough bleeding: random spotting and light bleeding that may happen when someone uses birth control to stop their period.
Breakthrough bleeding isn’t the same as having a period. It is usually less blood, for starters, and may not be accompanied by the symptoms you got during your period.
Still, it’s something Prager likes to inform people of so they can prepare for it. Breakthrough bleeding typically lasts, off and on, for three to six months after you have started period suppression. But, for some people, it can last longer or never fully go away.
Having some spotting doesn’t mean your contraceptive isn’t working or that something is wrong. It just means your body is adjusting to its new dose of hormones. Sometimes people may have to work with their doctor to find the right dose or type of contraceptive for their body.
“With Depo-Provera, someone might need dosing to be more frequent. So every 10 weeks instead of every 12, for example,” Prager says.
If breakthrough bleeding is interfering with your life, there are ways to try to stop it without full-on quitting using birth control, too.
This is easiest to do if you’re taking birth control pills, of course. You can stop taking the pills for three to five days, allow your body to have a withdrawal bleed, then start taking the pills again, according to Prager.
“Sometimes you just need to have the uterus shed its lining,” Prager explains.
If you have breakthrough bleeding that starts suddenly after you’ve been on birth control for a while, gets heavier or comes with other symptoms, it’s worth talking with your doctor about. It’s also worth a discussion if you’re using a hormonal IUD or a shot, as there may be some treatments that can help with the bleeding, Prager says.
“Depending on the situation, we never want to assume breakthrough bleeding is because of decreased action of the menstrual suppression, but instead always want to at least consider other causes it could be, like a polyp or fibroid or even cancer in the uterus,” she explains.
It’s worth noting that these things are less likely than your body just struggling to adjust to the birth control you’re taking — and that birth control lowers your risk for all of them. Still, better safe than sorry, right?
Does menstrual suppression cause infertility?
The short and complete answer is: No.
Assuming birth control and period suppression can cause infertility over time is a common misconception, Prager says.
“With almost all contraception there’s a relatively immediate return to fertility once someone stops using the contraception. It depends on someone’s baseline fertility level,” she explains.
That means that if you struggled with infertility prior to taking birth control, you’ll still have the same amount of difficulty after you stop taking it. If you haven’t struggled with infertility, birth control and stopping your period won’t change that.
Some birth control methods, such as the Depo-Provera shot, may cause a delay in returning to fertility that people may need to factor into their baby planning.
“That doesn’t mean it is decreasing future fertility, it just takes a longer time for it to leave the system. With Depo-Provera, I recommend someone stop six months before they want to try to conceive,” Prager says.
What if I want to get my period again?
First, some important information: If you want to take birth control and suppress your period for years to come, that’s totally OK.
“Frankly, if someone never wanted a pregnancy and never wanted to have a period, they could safely suppress menses from puberty to menopause,” Prager says.
If you’re wondering how you’d know you’re entering menopause if you’ve been suppressing your period, well, there are other ways to tell, such as if you start getting hot flashes or night sweats or are at an age where menopause typically starts).
If, however, you want to have a baby or aren’t enjoying the side effects from taking birth control, you may decide to start getting your period again, which is also totally safe.
There isn’t anything special you need to do to bring your period back other than to adjust or stop your birth control. If you’re taking pills, this means starting to take the week of inactive pills again. If you have gotten a shot or an IUD, it means not getting another shot or getting your IUD removed by your doctor.
It’s also important to recognize that, while your period may return exactly as it was before you stopped it, it may also change. You could get new symptoms or different period severity or duration than you had previously.
“Prepare for it to be as unpleasant or more than it used to be. It might be totally different from how people remember it. It’s important not to have expectations for what it will be,” Prager says.
Ultimately, if you get your period again and are miserable, it’s OK to go back on birth control and suppress your period again. The choice is up to you.

 Healthy ideas for your inbox
Healthy ideas for your inbox