People who have periods (or who suppress them with birth control) know that bleeding every month comes with a host of other unpleasant symptoms, like cramps and bloating. We also know that someday these things will (thankfully) end when we reach menopause.
But did you know that there’s a stage before menopause where more un-fun symptoms can occur? It’s called perimenopause, and not enough people talk about it.
What is perimenopause and when does it start?
Perimenopause is a life stage that starts when the eggs produced by your ovaries start dying off. (Fun fact: People with ovaries are born with all the eggs their body will ever create.)
Once the eggs leftover are not fertile and your ovaries stop releasing an egg each month (aka your period stops), you have reached the end of perimenopause, which is the beginning of menopause.
While the eggs are depleting, the ovaries are also losing their ability to produce hormones such as estrogen and progesterone — and this is why perimenopause can cause symptoms that may seem pretty random.
“These ovarian hormones also play a role in bone strength, skin integrity (especially in the vagina and urethra), sleep, mood, body temperature regulation, blood vessel function, sexual function, and cognitive (brain) function,” explains Dr. Ginny Ryan, division chief of Reproductive Endocrinology and Infertility at UW Medical Center – Montlake.
Perimenopause typically begins in someone’s 40s or 50s, but some people may enter it earlier due to chronic medical conditions like heart disease, having a hysterectomy or having an ovary removed. People who smoke or have a family history of early menopause are also more likely to enter perimenopause at a younger age.
There is a condition known as primary ovarian insufficiency, or premature menopause, which makes someone go into menopause much earlier. Additionally, having both ovaries removed sends someone immediately into menopause.
What are the signs of perimenopause?
One of the most obvious signs of perimenopause is period irregularities. This may start with periods coming more irregularly or not lasting as long and then progress to weeks and then months without a period.
These are normal signs of perimenopause; however, there are a few types of irregularities that warrant a talk with your doctor.
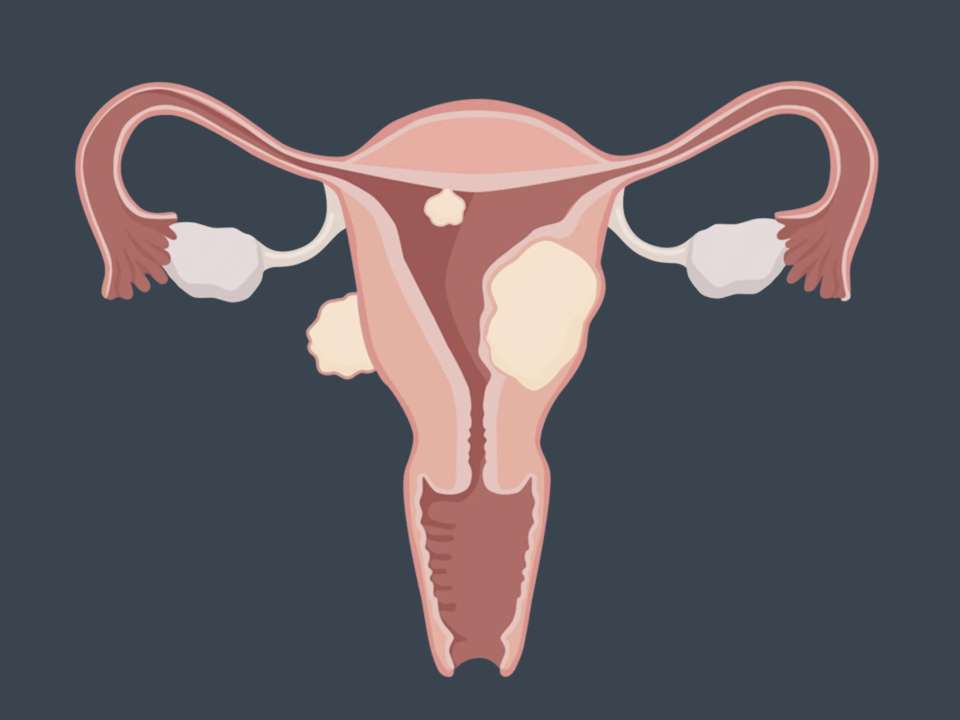
If you are getting periods more frequently or they’re lasting longer, or if you have spotting between periods, it could be a sign of something other than perimenopause, such as uterine fibroids or even, in rare cases, cancer. It’s a good idea to bring up any of these symptoms to your doctor.
Of course, being on birth control could also cause these changes. Pay attention to what is normal for your body while you’re using birth control and note if anything different starts happening.
Aside from changes to your period, there are a ton of other symptoms of perimenopause, many of which may sound like period symptoms or even menopause symptoms. Ready for the (long) list? Take a deep breath and here we go:
- Breast tenderness
- Hot flashes and night sweats
- Vaginal dryness
- Urinary incontinence
- Higher risk for UTIs
- Changes in sexual function and desire
- Fatigue and sleep problems
- Mood changes, such as anxiety or depression
- Worsening PMS symptoms: cramps, IBS, bloating, etc.
- Weight gain
- Hair loss
- Heart palpitations
- Dry eyes and skin
- Headaches
- Brain fog or trouble with memory or concentration
- Dry mouth or changes in taste
- Tingling in hands or feet or electric shock feelings
- Muscle aches or joint pain
- Worsening allergies
- Dizziness
That’s a lot, right? The good news is you probably won’t experience all of these. But as you progress through perimenopause, your symptoms may change, too.
“Every woman’s symptoms are different, and some women have few symptoms during this transition. Others may find the symptoms very disruptive to their quality of life and may seek care for these,” Ryan explains.
What if I’m on birth control or other hormones?
If you take birth control continuously to stop your period — or if you don’t bleed much anymore because of the method you use — you may wonder: How will I know when I start entering perimenopause if I’m not bleeding?
Just because you’re taking hormones doesn’t mean your body’s natural hormonal cycle isn’t still changing. But it does mean you may notice those changes less, Ryan says.
This may seem odd or may even be frustrating, but it comes with some good news: You may also be less likely to experience perimenopause symptoms.
If you’re taking hormones for other reasons, such as gender-affirming care, that will also change how perimenopause impacts you.
How can I treat perimenopause symptoms?
Most of the time, perimenopause symptoms can be treated in the way you normally treat mild ailments: pain relievers for headaches or joint pain, topical creams for dry skin or other skin changes, and so on.
If you’re experiencing mood or other mental health changes that are interfering with your life, it’s a good idea to talk with your doctor and consider either trying antidepressants or other medications or even making an appointment with a mental health specialist.
If symptoms are derailing your life, there are options. Hormone replacement therapy can help replace lost hormones and ease symptoms. This option isn’t for everyone, though, as for some people it can increase their risk for heart disease, stroke, blood clots or breast cancer.
It’s worth discussing any symptoms you’re having with your doctor, so you can go over your medical history and individual risk factors and find the best treatment options for your individual needs.
How long does perimenopause last?
Technically, perimenopause lasts until you enter menopause, so the exact amount of time varies. Some people may be in perimenopause only a few years; for others, it may last longer.
Once your period has been gone for a whole year, perimenopause is over and you’re officially in menopause.
Does perimenopause have long-term health impacts?
Perimenopause is a natural phase of life, but unfortunately it can put some people more at risk for chronic health problems. The main one? Osteoporosis, or bone loss.
The risk is highest for white people who smoke, are thin and are sedentary, Ryan says.
“Bone loss can cause significant problems such chronic pain, loss of height, and fracture, and this problem should be screened for by a physician routinely,” she adds.
If you’re concerned or are experiencing back pain — one common symptom — talk with your doctor about it.
Osteoporosis may not always cause symptoms, so often tests are needed to confirm a diagnosis. The main goals of treatment are to prevent further bone loss and ease any pain you’re having. Treatment options can include medications, exercising more, ensuring you get enough vitamin D and calcium, and limiting caffeine and alcohol.
Some good news for transgender and non-binary folks: If you’re taking testosterone, you’re less likely to get osteoporosis once you enter perimenopause, Ryan says.
It’s important to recognize that, while perimenopause can be difficult to deal with, it isn’t an inherently bad thing. It is a natural part of life that, while sometimes difficult or stressful, is ultimately leading you into the next chapter.

 Healthy ideas for your inbox
Healthy ideas for your inbox