Reproductive health issues often aren’t talked about enough — and uterine fibroids fall into that category.
Fibroids are very common and can affect anyone born with a uterus. One study found that by age 50, 70% of white women and 80% of Black women will have fibroids diagnosed. Approximately 30% will require treatment for severe symptoms.
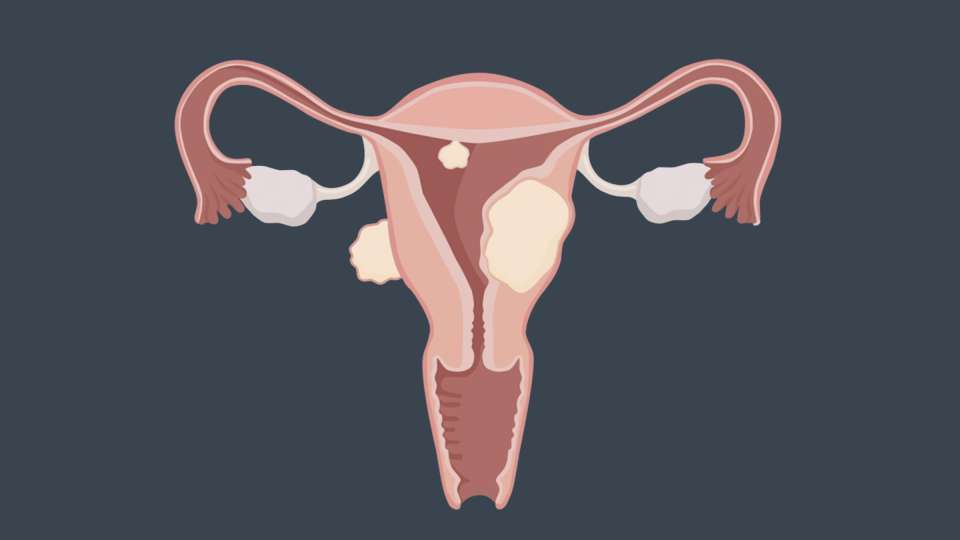
Uterine fibroids are benign tumors made up of muscle and connective tissue cells. Uterine fibroids are not cancerous. They can grow within the uterine wall, in the uterine cavity or on the outer uterine wall.
So, should you be worried if you’ve been diagnosed with fibroids? Should you have them removed? And how can you manage any symptoms they may cause? UW Medicine gynecologist Dr. Seine Chiang, who treats uterine fibroids and specializes in minimally invasive gynecologic surgery, has answers.
Q: What causes uterine fibroids?
Dr. Chiang: Despite how common fibroids are, we don’t know much about specific factors that regulate their development and growth.
We do know that each fibroid originates from the proliferation of a single muscle cell. Hormones such as estrogen and progesterone can cause fibroids to grow, and treatments aimed at suppressing these hormones can decrease fibroid size and symptoms. Environmental exposures that affect the way our genes work, access to care, and other social determinants of health likely all play a role, but exactly how is less clear.
Studies have noted that Black individuals experience earlier age of onset and greater disease burden versus white individuals. One study suggests that the prevalence of fibroids is three times greater in Black individuals and two times greater in Asian-Chinese individuals compared to white and Hispanic individuals.
While there is no clear cause for fibroids, there are a few things that research has shown to be associated with them, such as being premenopausal, never having been pregnant, a family history of fibroids, obesity, and environmental factors such as Vitamin D deficiency, smoking, drinking a lot of alcohol, a red meat-based diet and chronic stress. Getting your first period at a young age (before age 11) and experiencing menopause at a later age can also contribute.
Q: What are the most common fibroid symptoms?
Dr. Chiang: Many people with fibroids won’t have symptoms, or they may have vague symptoms, due to the slow growth of these tumors.
The rate of growth and location of the fibroid as well as the overall size of the uterus may determine if you have symptoms and what those symptoms are. Large uterine fibroid size (either a large fibroid or many smaller fibroids) may cause noticeable symptoms such as pelvic pressure, pain with sex, peeing frequently or the abdomen getting larger. Fibroids in the uterine cavity, even small ones, are more likely to affect your period, making the bleeding heavier or last longer or occur more frequently, even when the uterus is not enlarged.
Fibroids can also cause anemia due to blood loss; when diagnosing you with fibroids, your doctor can check for low iron or anemia with blood tests. Anemia doesn’t always cause symptoms; if it does, the symptoms may be subtle enough that you don’t notice them much. If you experience excessive bleeding during your period, this may become a medical emergency that requires immediate intervention to stop the bleeding.
Q: How are fibroids diagnosed?
Dr. Chiang: Studies suggest that up to 70% of individuals with fibroids have no symptoms, but this is an underestimation as fibroids tend to grow slowly and symptoms may develop gradually and be normalized by the patient. They may be experiencing vague symptoms that are not initially relayed to their doctor.
These “asymptomatic” fibroids are often detected incidentally on a pelvic exam or on an ultrasound or CT scan for other conditions. A pelvic exam where the uterus is felt to be enlarged may be the first indication that fibroids are present.
Individuals often feel relieved and validated to find out that there is an explanation for their symptoms and that there is treatment available. Based on national recommendations, routine pelvic exams are not medically necessary if the patient has no symptoms or medical conditions necessitating this uncomfortable exam. So fibroids are often detected when they are quite large or cause significant symptoms.
Individuals with symptoms suggestive of fibroids should have an exam of the abdomen and pelvis and a pelvic ultrasound. Additional tests should be based on ultrasound results, symptoms and management goals.
Q: I don’t have fibroid symptoms now. Will I develop any?
Dr. Chiang: It depends: The uterus size, fibroid location and rate of uterine enlargement often affect whether you are likely to develop symptoms. Since fibroids tend to grow over time, it’s possible you could get symptoms later even after you’ve had fibroids for a while.
If your fibroids are small and don’t cause uterine enlargement, they probably won’t cause symptoms — unless they’re in or near the uterine cavity.
For people with fibroids, it’s important to be seen by a healthcare provider periodically to review your symptoms, re-evaluate fertility plans, assess uterine fibroid size and review treatment options.
If you already have one fibroid, you could get more. Fibroids may grow or multiply, and fibroids within the same uterus may grow at different rates. While they won’t disappear on their own unless they are surgically removed, they do tend to shrink after menopause and with certain nonsurgical treatments.
Q: How are fibroids treated?
Dr. Chiang: There are lots of options for treating fibroids if they’re causing problems — and if they aren’t, you may not need to treat them at all.
If your fibroids are causing bleeding, discomfort or other symptoms that interfere with your life, you should definitely talk with your doctor about it. The size and location of the fibroids, along with what specific symptoms you have, fertility goals and feelings about uterine preservation will determine the best course of action for treatment.
All of the current fibroid treatment options have potential risks and side effects. We need more research to develop prevention strategies, and not just treatment.
The only cure for fibroids is surgery to remove the fibroid uterus or hysterectomy. Approximately one-third of all hysterectomies worldwide are for fibroids. There are several other types of surgeries such as myomectomy that can treat the fibroids causing the symptoms and are less invasive with quicker recovery than a hysterectomy. Myomectomy removes fibroids, preserves the uterus and leaves options for future fertility, though you may need a cesarean delivery for future pregnancies. Other treatment procedures include uterine fibroid embolization and radiofrequency thermal ablation of fibroids. However, the untreated fibroids may continue to grow and symptoms may recur.
Not everyone needs a procedure or surgery; instead, medical treatment can just target certain fibroid symptoms. Management of bleeding symptoms could involve taking non-hormonal or hormonal suppression of menstrual bleeding.
Nonhormonal nonsurgical options for treating bleeding include nonsteroidal anti-inflammatory medications such as ibuprofen or naprosyn. Alternatively, tranexamic acid tablets during the first 5 days of the period are also very effective in managing heavy periods, regardless of the cause. However, these medications do not shrink the fibroids.
Hormonal treatment options to treat bleeding include birth control pills, progesterone pills, progesterone IUD insertion or taking other types of hormonal medications to slow heavy menstrual bleeding and decrease blood loss.
There are medications that can treat the bleeding and shrink the fibroids by decreasing the estrogen and progesterone production by the ovaries but have side effects that mimic menopause and are not generally used for long-term management.
Q: Will my fibroids affect my fertility?
Dr. Chiang: Fibroids can affect fertility and pregnancy outcomes, but they don’t for everyone.
They can also increase the chance that, if you get pregnant, you may experience pregnancy loss, need a cesarean delivery, have pregnancy complications such as growth restriction in the fetus, breech presentation, bleeding, or your baby could be born preterm.
The best thing to do is talk with your doctor about your goals and what treatment options are available to you. And ask about how often you should get your fibroids checked and if you should be checked for anemia and low iron — this is how you can stay on top of any symptoms that may develop down the line.

 Healthy ideas for your inbox
Healthy ideas for your inbox





