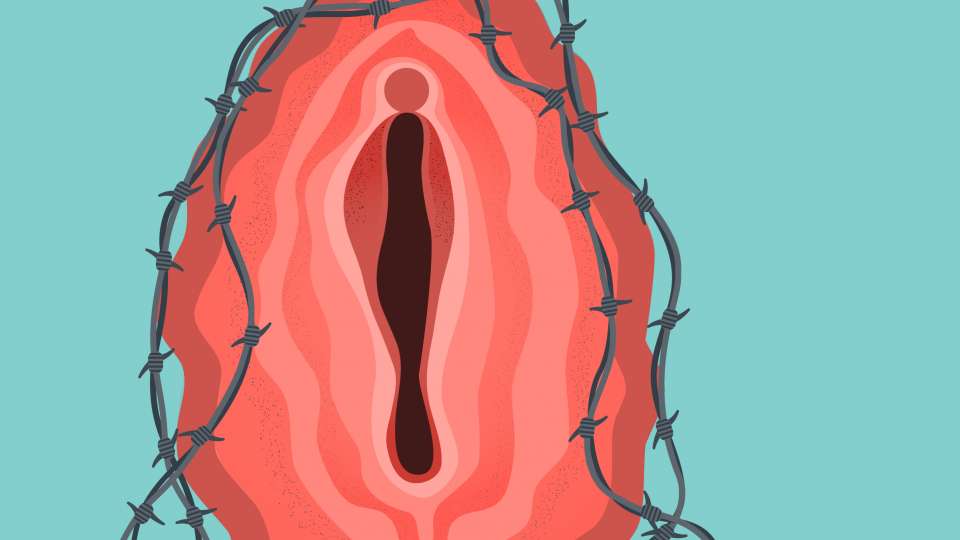
It’s date night, you’re in the mood and things are going great. But when you and your partner start to get intimate, you feel aches, cramps and even stabbing pain. What gives?
While not often talked about, pain during sex is common: According to the American College of Obstetricians and Gynecologists, nearly 3 out of 4 women experience pain during sex, called dyspareunia, at some point in their lives.
There are a lot of different reasons women experience this pain, ranging from a lack of lubrication to larger reproductive system issues.
“If a woman comes in and is experiencing acute pain during sex, it gives us a chance to check for treatable causes of the pain,” says Dr. Anna Kirby, a board-certified obstetrician-gynecologist who sees patients at the Pelvic Health Center at UW Medical Center – Northwest.
To help you understand any itching, burning or tenderness, Kirby explains common factors and conditions that might be causing your discomfort during sex — and how to treat them.
Infections and painful sex
Infections are common culprits of pain during sex and are easily treated with medication, so it’s best to test for an infection first and then move on to other factors that might be causing your pain, Kirby says.
Yeast infections, urinary tract infections (UTIs) and sexually transmitted infections (STIs) can cause itching and burning during sex, inflammation, unusual odor and gray or creamy discharge, depending on the type of infection.
But just because you notice a fishy odor doesn’t mean you should self-diagnose and head to the drug store for antibiotics.
“A lot of patients empirically get treated for bladder and vaginal infections without a proper evaluation,” Kirby says. “My concern there is they are getting a lot of unnecessary or mis-directed antibiotics and treatments.”
This is problematic because sometimes these symptoms are not caused by common vaginal infections, and if the discomfort persists, it can lead to pelvic muscle spasms, sensitive nerves and inflamed skin — all of which can cause pain during sex that persists even without an infection present.
Plus, it’s especially important to check in with your doctor so you can receive treatment for more serious infections like pelvic inflammatory disease (PID), which can cause scarring and infertility if left untreated.
Pre- and post-menopausal factors and painful sex
Hormones are another common cause of pain during sex, and they can affect women before and after menopause.
For women who have gone through menopause, lower estrogen levels can lead to vaginal dryness or atrophic vaginitis, a thinning of the vaginal lining. If you have atrophic vaginitis, it can cause discomfort during penetration, an itching or burning sensation, and light bleeding after sex.
While less common, younger women with a history of taking birth control pills can also experience a thinning of the vaginal lining.
“For a small percentage of those who take the pill, it makes the lining of their vagina thinner like it would be after menopause, even though they are young and have a normal amount estrogen in their body,” Kirby says.
Whether you’re experiencing dryness or a thinning of the vaginal lining, she notes that a topical vaginal estrogen can help with lubrication and decrease any friction or pain. For younger women, other topical hormones, like testosterone and androgens, can also help.
Muscular factors and entry pain during sex
If your pain is most intense during deep penetration — especially if you are experiencing this pain in non-sexual scenarios, like when you use a tampon — it might be caused by pelvic muscle spasms, sometimes called vaginismus, or pelvic floor spasms.
“If pelvic muscles go into spasm and can’t relax, it can cause symptoms similar to vaginal infections as well as cause pain with vaginal penetration,” Kirby says.
These muscle spasms can feel like a deep cramping pain or sharp stabbing pain during sex, and it may also feel like your partner is meeting resistance during penetration.
The best way to treat muscle spasms and relax your pelvic floor is working with a pelvic floor physical therapist.
In the event that you’re still experiencing pain, your doctor can inject the muscles with an anti-inflammatory to make them less tender or Botox to temporarily and partially paralyze the muscles.
Anatomical factors and deep pain during sex
If your pain is persisting outside of sexual encounters and seems related to your menstrual cycle, it might be caused by endometriosis, Kirby says.
Endometriosis is a disorder where the tissue that typically lines the uterus grows outside of the uterus, often on other pelvic organs. This tissue then breaks down, causing severe, prolonged pain in your back, pelvis and abdomen.
The good news? There are treatments available that can help relieve discomfort through medications, hormone therapy and surgery.
On the flip side, if your pain comes on suddenly and intensely during sex, it may be caused by a different anatomical factor: ovarian cysts, or fluid-filled sacs on your ovaries.
While many women develop ovarian cysts, only about 8% of premenopausal women will develop cysts that cause pain and require treatment. And for a very unlucky few, these cysts rupture.
If you experience immense, sudden pain, seek medical treatment immediately.
While most ovarian cysts go away on their own, your doctor can prescribe birth control pills to reduce the formation of additional cysts and they can be removed surgically in the case of ruptures or other complications.
Finally, if your pain is concentrated in your vulva, you may be experience vulvodynia, a chronic pain in your vulva and the entrance of your vagina.
“First you always want to evaluate with a physical exam,” Kirby says. “There are a lot of treatments that help, like steroids and hormones.”
Another way to soothe irritation and any external rubbing pain is to apply a topical anesthetic, like lidocaine, to the area where your vulva connects to your vagina. For some women, it helps to apply this topical anesthetic before sex.
Emotional factors and painful sex
Along with physical factors, emotional and psychological factors can contribute to discomfort during sex — even when you are in a healthy, consensual situation.
“If you don’t have a supportive partner, if you have a history of abuse, or there is something else stressful going on, it can make sex uncomfortable,” Kirby says. “Sex is a really emotional process. Things like arousal and lubrication have so many factors at play, including emotions.”
Kirby recommends speaking with sex therapist, who is a trained healthcare professional who can help you deal with stressors as they come up. You can also work with a mental health professional to help you move through any past trauma that may be causing your discomfort during sex.
When to seek medical care for painful sex
There are a lot of reasons you might be feeling pain, and it’s hard (and unwise) to diagnose these at home.
“It’s a really stressful thing. Whatever the reason sex is painful, it can be remarkable stressful for a patient and their partner,” Kirby says.
While it may feel uncomfortable to talk about sex with your doctor, try not to suffer in silence. If you’re feeling pain, a quick checkup could mean improving your reproductive health and treating any issues that are causing discomfort during sex.
Soon you’ll be back to date night — sans discomfort.

 Healthy ideas for your inbox
Healthy ideas for your inbox





