So you’re hooked on HBO’s viral new show “The Last of Us” about a mutated type of fungus that turns humans into zombies.
The premise may seem far-fetched, but in reality, it hits a little too close to home. Sure, fungi can’t turn people into zombies (yet), but a type of Cordyceps fungus can do that to ants by hijacking their brain and nervous system.
And did you know that fungi kill thousands of people each year?
How serious are fungal infections?
Mushrooms are having a moment. Psilocybin, a compound extracted from some mushrooms, is increasingly being studied as a therapy for people with anxiety, depression and other types of mental illness.
Rather than therapeutic, though, some fungi are dangerous. And while a fungal infection won’t turn you into a clicker — or, worse, a bloater (ew) — it can be life-threatening.
“Fungi don’t control human behavior in any directed way. They don’t require any further evolution to be dangerous to us,” says Dr. David Fredricks, a professor of medicine at the University of Washington School of Medicine and a researcher who studies microbial communities at Fred Hutchinson Cancer Center.
There’s Cryptococcus neoformans, which can cause pneumonia — and meningitis, a symptom of which, eerily enough, is behavior changes. There’s Mucormycosis, which can affect the skin, brain, lungs and gastrointestinal tract.
Then there’s invasive Candidiasis, caused by the same fungus that causes yeast infections and thrush. It is a top cause of sepsis or bloodstream infection, as well as a top cause of prolonged time spent in the hospital.
More common types of fungal infections, however, are mostly harmless (though annoying). For example, vaginal yeast infections and oral thrush — a white coating on the tongue — are both caused by fungi.
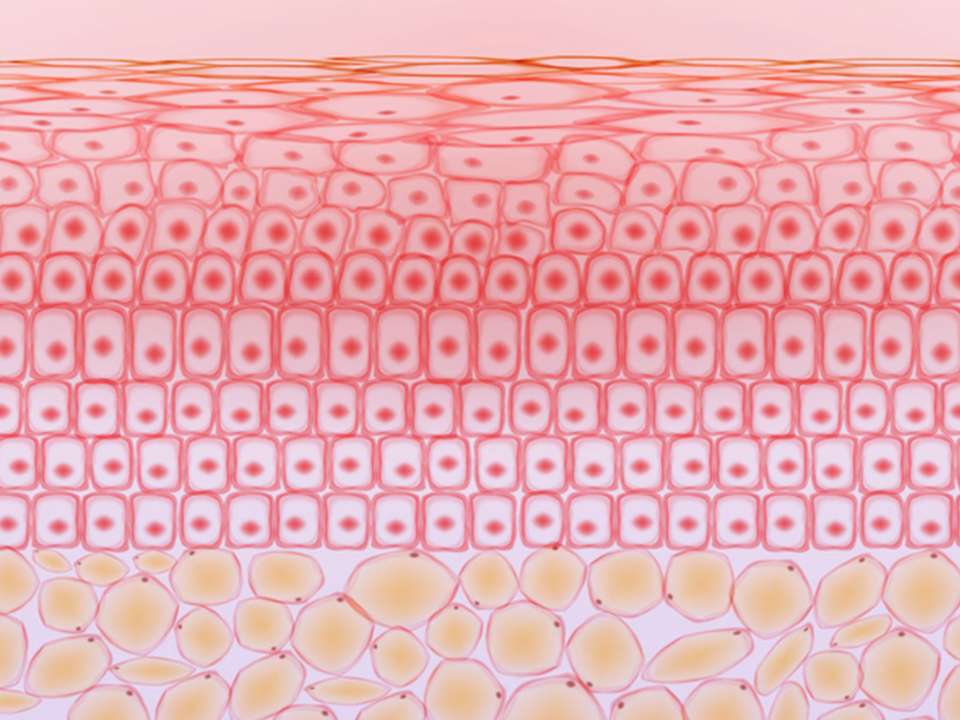
Fungal infections can also occur on the skin, hair and nails but are usually easily treated with antifungal medication that you take or an ointment that you apply to the affected area.
How does someone get a fungal infection?
Yeast infections, thrush and other infections that occur on the skin or in mucous membranes happen because of fungal overgrowth. Yeasts and other types of fungi live in our bodies — even in the gut, in colonies sometimes called a mycobiome (just like the gut microbiome). Normally, these fungi are harmless to us and only cause harm if their numbers grow too large.
More serious internal infections happen when someone inhales fungal spores.
“These infections frequently start in the lungs or sinuses and are carried into the human body from the air, where they can initiate infection and then spread to other sites including the brain,” Fredericks says.
Research has shown that most of us inhale anywhere from thousands to tens of billions of fungal spores every day. Yet, most of the time, they won’t make us sick. Why? Our immune system protects us.
But this isn’t the case for everyone. People who are immunocompromised in some way, such as from a chronic condition like diabetes, undergoing cancer treatment or receiving an organ transplant, are at higher risk for internal fungal infections.
Will fungus evolve to be deadlier?
The likelihood of a type of fungus mutating so rapidly it turns most of us into zombies and creates worldwide societal collapse in a single day is, well, basically impossible. Even infectious agents that mutate rapidly, like antibiotic-resistant gonorrhea, don’t have that kind of power.
However, it is possible that fungi that already impact human health could evolve to be deadlier thanks to climate change.
Valley Fever, an infection caused by Coccidioides immitis, has been found in Washington state soil and in other locations throughout the world. Cases of Valley Fever are increasing and could continue to do so thanks to warmer, wetter weather (and warmer, wetter soil) caused by an increase in temperature and rainfall due to the warming planet.
So-called superfungus Candida auris first appeared on the radar in 2013 and has since caused deadly outbreaks and thousands of infections throughout the United States. Climate change could make it easier for these outbreaks to happen, but another problem is the fact that the fungus has evolved rapidly to resist all existing antifungal treatments.
It’s not something to panic about yet, but it’s something to be aware of — especially since there are currently no vaccines. There are, thankfully, effective antifungal treatments that reduce the burden of fungal disease, though as fungi continue to develop resistance to these drugs, their usefulness may change.
Are fungal vaccines in the future?
Speaking of fungal vaccines, why don’t they exist? After all, we know how helpful vaccines are at preventing serious illness and death.
There are challenges to creating a vaccine to target fungi. For one, vaccines are most helpful in people who have strong immune systems, so even if a vaccine can be developed, they may not be as helpful to someone who is immunocompromised.
And since fungus and humans share a lot of DNA in common, creating a vaccine to target fungal cells could accidentally trigger a strong autoimmune response in the body, where the immune system starts attacking healthy human cells.
Several antifungal agents are currently being studied and proving effective, with some even being studied in human clinical trials.
For now, all we can do is wait — and endure and survive, of course.

 Healthy ideas for your inbox
Healthy ideas for your inbox