Having lingering effects from COVID-19, a medical condition called long COVID-19 or post-COVID-19, is disheartening — literally. Not only can symptoms like shortness of breath, chest pain and heart palpitations be hard to handle mentally and physically, but they can also indicate that the virus has taken a toll on your heart health.
Research has shown that people with post-COVID-19 are more than twice as likely to develop heart issues. Even without longer-term symptoms, getting COVID-19 can put someone at risk for things like stroke or heart attack up to a year after infection.
So how do you know if you have heart issues from post-COVID-19? And how do you resolve them?
The most common post-COVID-19 heart symptoms
At this point, we all know how varied people’s experiences of COVID-19 can be. Some get really sick while others don’t even know they have the virus.
The same is true with how COVID-19 affects the heart. Most people won’t get post-COVID-19 or have any heart issues, but it’s estimated that 1 in 13 people will have symptoms — ranging from brain fog and fatigue to joint and muscle pain to lung and intestinal problems — that persist longer than three months, according to the Centers for Disease Control and Prevention (CDC). Among those, up to 29% will have heart symptoms after they recover from initial COVID-19 infection, says Dr. Anita Chopra, a UW Medicine family medicine specialist who works with patients who need post-COVID-19 rehabilitation.
“The patients we see in the clinic were never hospitalized; many developed COVID-19 years ago and are still having lingering symptoms,” she says. “Most patients I’ve seen did not have any cardiovascular disease history before they developed COVID-19.”
The most common issues she sees are:
- Tachycardia, which is an elevated heart rate (above 100 beats per minute)
- Other types of heart palpitations
- Shortness of breath
- Postural orthostatic tachycardia syndrome (POTS) which causes someone’s heart rate to spike and blood pressure to drop when they sit or stand up
What COVID-19 can do to your heart
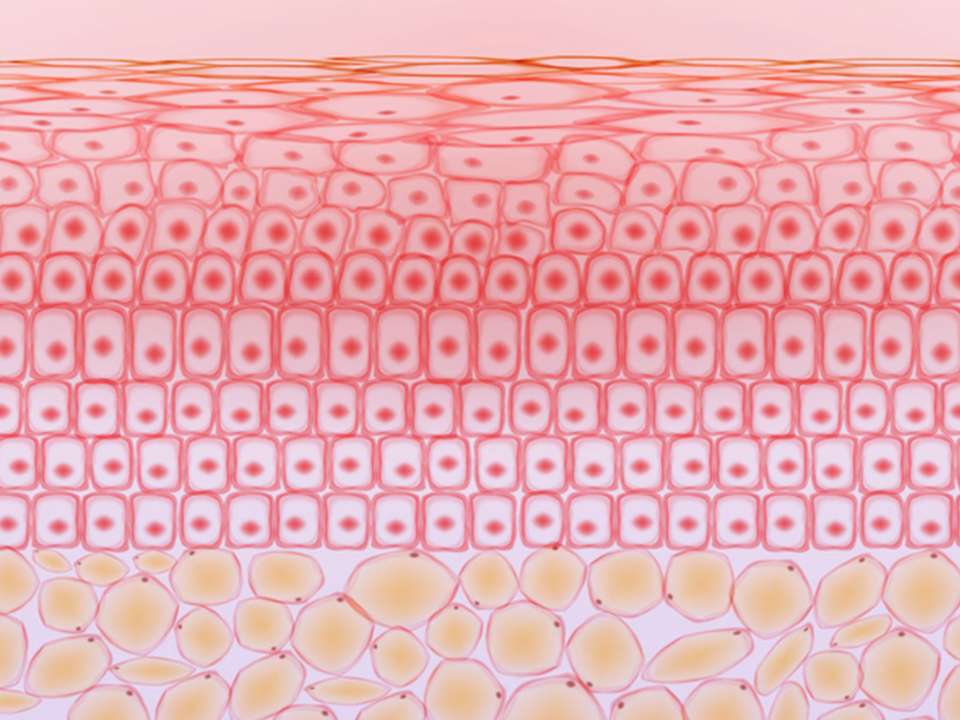
But how does a respiratory virus lead to these sorts of things? It’s well-known now that COVID-19 can cause acute (aka short-term) heart issues such as myocarditis, which is inflammation of the heart muscle, and cardiomyopathy, which is weakening of the heart muscle. This can put people at risk for things like a stroke or heart attack, typically for up to a year after initial COVID-19 infection.
Longer-term, the virus can cause chronic inflammation throughout the body, including the heart, says Chopra. Research suggests that chronic inflammation triggered by the virus could increase the risk of cardiovascular disease, including stroke and heart attack.
Yet there are other theories, still being studied, that may further explain why some people have such lasting symptoms: The virus itself may linger in the body and attack healthy tissues; the presence of the virus may trigger an exaggerated autoimmune response, with the body essentially attacking itself; and the virus may cause small blood clots, or microclots, to form, restricting blood flow and damaging blood vessels.
How to know if you have post-COVID-19 heart problems
To determine if heart symptoms are due to long-COVID, many tests may be needed. Fortunately, most of these tests are simple: they include things like blood tests, wearing a heart monitor to look for heart rate abnormalities, having an echocardiogram to look at the condition of the heart.
Often, these tests are normal. When that’s the case, patients are often referred to a post-COVID-19 specialist like Chopra.
What treatments work for post-COVID-19
“There is a lot of fear, a lot of anxiety, so that’s why I reassure patients that we have seen people getting better, though it may take time,” Chopra says. “The good thing is, symptoms like heart palpitations and dropping blood pressure are the first to start getting better.”
Treatment ranges from at-home remedies like staying hydrated, eating more salt and wearing compression socks, to working with rehabilitation specialists, physical therapists and cardiologists. Medications can help maintain a normal heart rate and blood pressure, plus help with anxiety.
Research suggests that some post-COVID-19 patients may have lower serotonin levels, so treating them with selective serotonin reuptake inhibitors (SSRIs) can help with anxiety and stress which, in turn, can help with heart issues.
Chopra also works with patients on what she calls the four P’s:
- Pacing: Limiting daily activities so you don’t exhaust yourself or trigger worse symptoms
- Prioritizing: Deciding what absolutely needs to get done each day versus what can be rescheduled or postponed to conserve energy
- Positioning: Modifying activities to make them easier and less likely to trigger symptoms
- Planning: Making sure to plan each week ahead of time and building in times for rest
The future of post-COVID-19 care
While post-COVID-19 heart problems (and other health issues) can be scary and overwhelming, you don’t have to suffer in silence; help is available. If your doctor doesn’t take your concerns seriously, see if you can go to a different doctor or get a second opinion. A lot is still unknown about post-COVID-19, but your symptoms are real and can be treated.
Chopra notes that the idea that a virus can cause widespread disruption to bodily systems is not new, though still not well understood. Doctors have known for a while that infection with Epstein-Barr virus can, in some people, lead to chronic fatigue syndrome.
“Right now COVID and long COVID have opened doors to understanding how viruses act and how they can make long-term changes in our bodies,” Chopra says. “I hope this will open a door to new studies and guidance on the lingering effects of viral infections.”

 Healthy ideas for your inbox
Healthy ideas for your inbox