Jasmine was a healthy young woman just starting out at the University of Washington when she fell down a set of stairs near the Intramural Activities Building (IMA).
“It was a long, steep set of stairs but, normally, I would have just brushed myself off and forgotten about it,” says Jasmine.
But the next day, she couldn’t straighten her right arm. One week later, she still couldn’t straighten it.
“It was just stuck. I kept blaming it on the fall, but then it didn’t get better,” says Jasmine.
Then her left elbow started hurting, too, though she hadn’t injured it when she fell.
“I blocked a lot of my memories from that time because I was in so much pain,” says Jasmine.
Recognizing symptoms of rheumatoid arthritis
“Jasmine was experiencing the onset of rheumatoid arthritis,” says Anders Peck, M.D., a rheumatologist at The Seattle Arthritis Clinic at Northwest Outpatient Medical Center and Jasmine’s doctor.
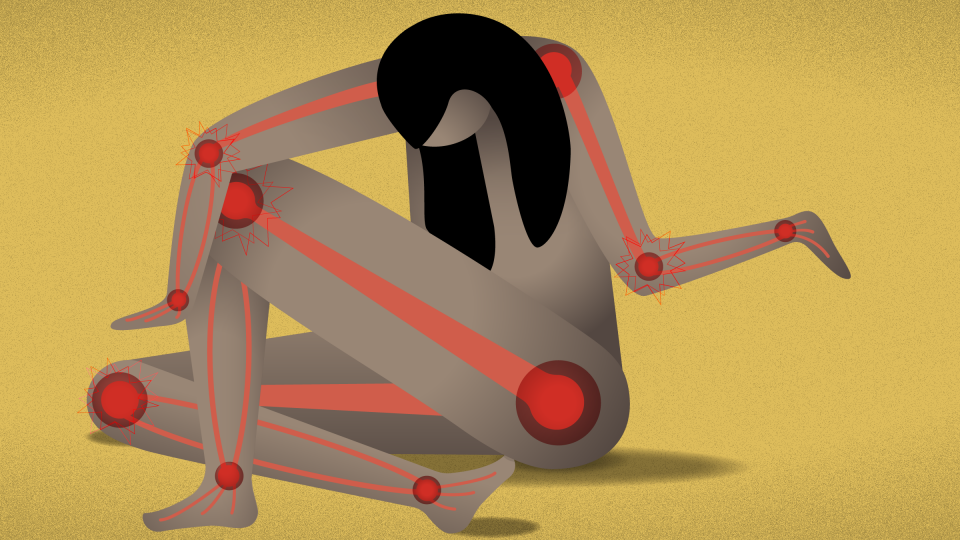
“It’s not like one day you wake up and everything is terrible, but severe pain and stiffness can start and worsen over a course of several days to a week. People might notice significant stiffness in the morning and swollen joints without any mechanical trigger. They may find that they have difficulties doing simple things such as lifting a coffee cup, writing or buttoning a shirt,” says Peck.
Symmetrical joint swelling is also an identifying characteristic of rheumatoid arthritis. The pain and inflammation that started in Jasmine’s right elbow joint and then affected her left elbow is a classic manifestation.
It’s best to go to a doctor on the early side of recognizing symptoms such as these.
“It’s important to treat rheumatoid arthritis early after it starts. It is an autoimmune disease and may be easier to treat before the immune system becomes established in an abnormal pattern. Early treatment also helps to prevent the likelihood of severe damage to the joints in the future,” says Peck.
But it can sometimes be challenging for young women who are otherwise healthy to recognize what they’re experiencing as symptoms of a disease.
Jasmine’s pain and stiffness worsened and spread to other joints — first her hands, then fingers, then knees. It was only a matter of weeks until the pain was excruciating.
Because she’d always been healthy, she figured that she would soon return to normal. Besides, she needed to focus on school. She put off going to the doctor and blocked the pain as best she could.
“I would take a lot of really long, hot showers. And I would sleep,” says Jasmine.
These were Jasmine’s only brief respites from pain. But to get to sleep, Jasmine had to cry herself there.
“While I was crying myself to sleep, I would curl up and try not to move because anytime I moved, it hurt,” says Jasmine.
What finally brought Jasmine in to see a doctor was another tumble, this time in her bedroom.
“I was getting ready for school one morning. My knees were so swollen that my jeans wouldn’t fit over them. I was trying to force my legs into my jeans when I fell over. That was it for me. I realized I just couldn’t do this anymore,” says Jasmine.
Initial diagnosis and treatment
If a primary care physician doesn’t refer a patient like Jasmine to a rheumatologist — the type of physician who treats systemic autoimmune conditions such as rheumatoid arthritis — the diagnosis can be missed. But in this way at least, Jasmine was lucky. She was referred to a rheumatologist.
“There are blood tests that can help to confirm a diagnosis of rheumatoid arthritis in most patients. Because some patients may not have a positive test, it is still very important for people to be evaluated by a rheumatologist with a detailed medical history and physical exam,” says Peck.
Typically, people are in their 60s when they develop symptoms of rheumatoid arthritis. But women tend to develop the disease at a younger age than men. They are also three times more likely than men to develop the disease.
Once diagnosed, treatment for rheumatoid arthritis is two-pronged: controlling the occasional flare-ups or periods of increased disease activity characteristic of rheumatoid arthritis and managing the long-term course of the disease. Rheumatoid arthritis is a systemic disease, meaning it can affect not only the joints but the entire body over time.
“It is common to start steroid medications such as prednisone to immediately control symptoms, but it’s not a good long-term medicine, so we use it cautiously,” says Peck.
Prednisone can have uncomfortable side effects such as fluid retention, acne and mood swings. But it suppresses the immune system, thereby helping to control a flare-up.
Most patients arrive at a rheumatologist’s door during a flare-up, when joints are actively painful, stiff and swollen. This was the case with Jasmine.
“It’s overwhelming at the start. I was in intense pain and then, suddenly, I had a diagnosis for this disease I’d never heard of. And because I was on prednisone, I didn’t even feel like myself,” says Jasmine.
Trial and error to pinpoint the best treatment
Finding the right medications to treat rheumatoid arthritis is challenging on several fronts. Because immune systems vary from person to person, a medication that works for one patient may do very little for another. Additionally, a drug that might work well for some time can suddenly stop working.
“There are researchers looking into personalized medicine in rheumatology, but in the meantime, we go through the smorgasbord of treatment options available in a way that makes sense in the context of a patient’s symptoms and other medical issues,” says Peck.
Insurance coverage also influences the choice of medications. A new tier of drugs known as biologics has transformed treatment of rheumatoid arthritis, but the drugs are prohibitively expensive; most insurance companies require patients to try less expensive options first.
Biologics are drugs that replicate naturally occurring substances, such as proteins, antibodies or hormones. For example, a vaccine is a biologic.
When the medications that Jasmine tried did not adequately relieve her symptoms, Peck recommended a biologic treatment for Jasmine.
“The biologics work by suppressing the immune system in a variety of ways. Since the immune system is inappropriately active in patients with rheumatoid arthritis, most of our treatments dampen the immune response,” explains Peck.
Biologic treatments for rheumatoid arthritis are administered by either injection or IV. Jasmine receives hers through an IV drip that takes six or seven hours to administer. She gets two infusions, two weeks apart — once every six months.
The treatment improved her symptoms dramatically.
“Sometimes now I even forget I have rheumatoid arthritis,” Jasmine says.
Living as a young person with a chronic illness
Managing a chronic illness on top of the already-significant stresses of young adulthood is no walk in the park. Jasmine has developed strategies to help her get through the day-to-day realities of rheumatoid arthritis while keeping her outlook positive.
“I wouldn’t say that I limit my activities, but I have to be more mindful. More planning has to go into things, and I have to think carefully about how to allocate my energy,” says Jasmine.
Peck says that patients with rheumatoid arthritis have to think about their health and healthcare in a way that most people in their young 20s don’t.
Another strategy of Jasmine’s is to stay on top of her preventive care.
“I see a massage therapist, and I’m going to start some hand therapy, too. Have you seen those gnarly pictures of people whose hands are stuck? That’s not what I want for myself,” says Jasmine.
Jasmine attended a support group for a while but decided against continuing with it. She discovered her own best medicine.
“For me, staying social was hugely important. I wouldn’t have been able to do it if I didn’t have my family and my friends to support me,” says Jasmine.
She has a piece of advice for anyone else suffering from an autoimmune disease, especially at such a young age:
“Find a way to continue to do the things you love even if you have to change it up a little bit. Because that’s one thing that really helps to keep your spirits up,” says Jasmine.
“Don’t get so focused on your disease that you forget to live your life.”

 Healthy ideas for your inbox
Healthy ideas for your inbox





