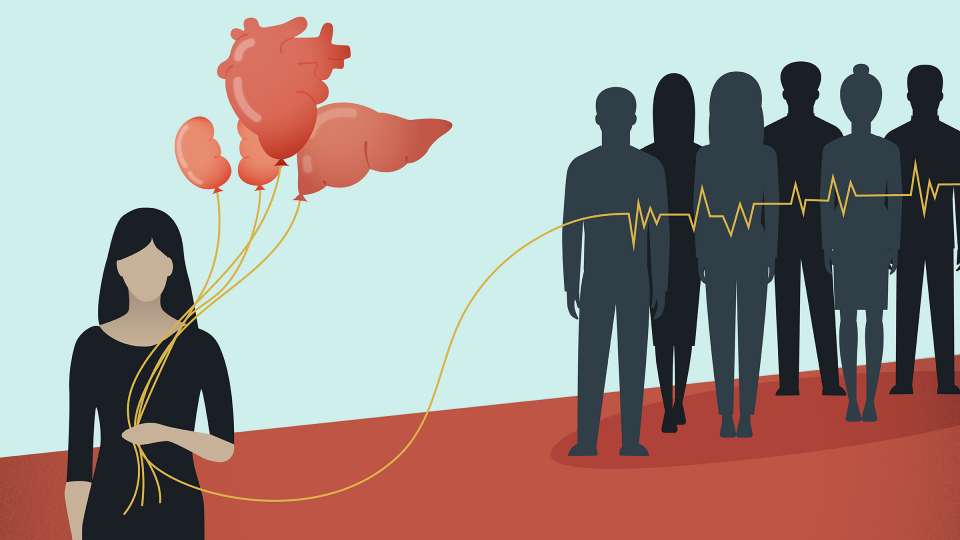
That little red heart on your driver's license is small but mighty. It means you're an organ donor and, seriously, thank you for that; you're a lifesaver, literally. Around 20 people die each day waiting for an organ transplant, and there were more than 113,000 people on the wait list as of January 2019.
“One organ donor can save up to eight lives through transplantation; one can save many more through tissue donation,” says Cate Oliver, communications program manager at LifeCenter Northwest.
Whether you’re a registered donor or not, maybe you’re wondering about how the process works. What exactly will happen to your organs after you die? And how do doctors determine who will get them?
Organ donation vs. tissue donation
When most people think of organ donation, they’re thinking about hearts, livers and lungs. But tissue donation, which includes things like bone, corneas, heart valves and even skin (your skin is your largest organ, after all) is actually much more common.
That’s because it’s much easier to preserve tissues than maintain whole viable organs, says Oliver.
“In order to be eligible to be an organ donor, someone has to be on ventilated support in a hospital when they die, to keep oxygen and blood flowing through the organs. Tissue donation is a little bit different: you don’t have to die in a hospital or be on ventilated support, but there’s a 24-hour window between time of death and tissue donation,” she says.
Tissue donation means you’re helping many people, from patients with burns who need skin grafts to children who need new heart valves to people who would need to have a limb amputated if not for a bone graft.
Among registered donors, few will die in a way that allows preservation of their organs for transplant. According to Oliver, fewer than 1% of deaths in the United States can result in organ donation.
Most organ donors became donors by dying from a traumatic injury, typically, to the head, or from severe brain injury due to a stroke, says Dr. Stephen Rayhill, a transplant surgeon at University of Washington Medical Center.
It’s also important to note that organ and tissue donation are different from whole-body donation, where someone specifies in their will that they wish all of their remains to be donated for use in medical school training or research.
Most people die of old age, but there is a small chance that a person could die prematurely and save others’ lives by becoming an organ donor. That is why people are encouraged to sign their organ donor cards and make their wishes known in case a tragic injury happens.
“None of us know how we’re going to die. The more robust the list of donors is, the more patients in need will get a transplant,” Oliver says.
How death is determined
If you’re a horror fan or connoisseur of those tabloid headlines about people who miraculously wake up after years in a coma, it might seem like death is somewhat of a nebulous concept.
While it’s true that people can recover from near-death experiences or be revived after their heart stops beating, death is pretty unmistakable in the world of organ donation.
“There are two ways to establish that someone is dead. One, via the age-old technique of demonstrating that there are no signs of life, no heartbeat, no breathing, no brain function, no blood flow. The second way, established more recently, is via the diagnosis of brain death, where a person can be declared dead when there is an absence of any brain function,” Rayhill says.
Brain death is a term thrown around in medical dramas on TV and is often misused or misinterpreted, so let’s be clear: Someone cannot spontaneously recover (or recover at all) from brain death. It is irreversible, unlike a coma, and there are specific guidelines doctors must follow in order to declare it.
Rayhill is aware of concerns that people might have and wants to offer reassurance that doctors won’t remove organs from a person who still has a chance to recover.
What happens after brain death is declared
After someone is declared brain dead, the organ procurement team is notified and they discuss the options with the person’s family.
According to Washington state law, if you are a registered organ donor, your wishes cannot be overridden by family members.
The transplant surgeon and representatives from the procurement team will talk with the family and answer any questions they have. Then, after all the required pieces are in place, the person will be transported to an operating room, where, respectfully, the organ procurement will occur.
How organs are procured
When a patient is dying and is a candidate for organ donation, the hospital contacts the procurement team to let them know that they might be needed.
Only after death is declared is the transplant team allowed to enter the operating room and retrieve the organs. They will only do so in accordance with the donor’s wishes, which means that if the donor was an organ but not a tissue donor, the teams will only retrieve organs, not tissues like corneas.
“In most instances when someone is eligible for donation, it’s probably an unexpected death; aneurysm, stroke, severe head injury. The family is in shock and having to think about donation on top of that is a lot. Our team is trained to help them take care of themselves, reminding them to sleep and eat and keeping them in the know and that they’re in control of what’s happening,” Oliver says.
The procurement process may seem methodical or a bit cold to some people, but Rayhill wants people to understand that everyone involved in the procurement and transplant process understands how difficult it is for the person’s loved ones — and how big of a gift the person is giving.
“There has to be a lot of respect paid to the donor. I always say a prayer or thanks or something for the donor if I’m there,” Rayhill says.
How transplant organs are preserved
Different organs require different levels of preservation in order to be eligible for transplant. Some organs, such as the heart and lungs, have a shorter window of time in which they can be preserved for transplant. Others, such as liver and kidneys, can be preserved for longer.
Organ preservation involves keeping the organs cold until they can be transplanted. High tech methods can be employed to further support the organs such as pumping organ preservation solution through the organs.
Even newer technologies like the “heart in a box” and “liver in a box” are being studied to further improve preservation of the organs. These devices provide oxygen and nutrients to the organs, maintaining blood flow to keep the organs warm and functioning.
Doctors are also finding ways to use organs that typically would be deemed unsuitable, like hearts from donors who tested positive for hepatitis C.
How transplant recipients are found
If the process of finding a potential donor match within the small window of opportunity when organs are still viable seems like a complicated process, that’s because it is.
Hospitals and procurement teams work with a national organization, the United Network for Organ Sharing, that helps match recipients with potential donors. Their database includes detailed information about both donor and recipient — things like blood type, weight and height, what geographic region they’re in and more. A computer system then matches the organs to the recipients.
“Once they’ve identified a few matches, they get the top matches from the list for every organ that is viable,” Oliver says.
After doctors determine the best match, the procurement team works to help get the organ to the recipient’s location. Since some matches cross state lines, this can mean that someone from the team drives or flies to a different region and accompanies the organ back to the hospital where the recipient will go for transplant.
Donor family care teams offer long-term support for donor families as well as for recipients. If desired, they also help facilitate correspondence and meetings between donor families and recipients.
“It’s really nice to see that something beautiful can come from such a tragic event,” Oliver says. “It helps a lot of families find healing.”

 Healthy ideas for your inbox
Healthy ideas for your inbox





