Your Body on Birth Control: How The Pill and Other Contraception Really Works

Everyone knows how condoms work, but if you use any other type of birth control it may feel like a leap of faith. You pop a pill, insert a ring or get an IUD and by way of some sort of scientific magic, you don’t get pregnant. Are you wondering what’s actually going on inside your body to make that process work? Or how one birth control method differs from another? We talked with Elizabeth Harrington, M.D., an obstetrician-gynecologist at the Family Planning Clinic at UWMC-Roosevelt in Seattle, to get the scoop on what’s going on behind the scenes in your body with eight of the most common forms of birth control.
Combined Hormonal Birth Control

The Combination Pill
Combined oral contraceptive is a daily method that contains low doses of estrogen and progestin—a synthetic form of the hormone progesterone. The pill, of which there are dozens of brands on the market, prevents pregnancy by stopping ovulation from occurring, says Harrington.
Naturally, two glands in your brain that control the reproductive endocrine system talk to your ovaries, telling them when to release an egg. When an egg is released, estrogen levels fall and progesterone levels rise, preparing the uterus for pregnancy. If an egg doesn’t get fertilized after ovulation, progesterone levels will dip back down, sending a signal back to your uterus and your brain that it’s time to move on to the next phase of the menstrual cycle. Estrogen production picks back up and the cycle repeats itself in a negative feedback loop, where “one hormone affects the other affects the other,” explains Harrington.
“When you’re taking the pill, your pituitary gland is getting the message that it doesn’t need to try to grow that egg; to not go through the usual cycle of hormones,” she says. “Your pituitary gland thinks you’ve already ovulated. That’s why if you miss pills at certain times of the month an egg can kind of squeak through, and then you can get pregnant.”
A 28-day pack contains three weeks of active pills and one week of inactive, reminder pills that cause you to have a monthly “withdrawal bleed” that seems like a normal period but doesn’t actually have any medical purpose, shares Harrington. When you aren’t taking hormones, your uterine lining will thicken throughout your cycle to prepare for pregnancy, and is then shed in a menstrual period if you don’t get pregnant. Since your hormone levels don’t fluctuate in the same way as they naturally would when you’re on the pill, your uterine lining doesn’t become as thick or need to be shed. The withdrawal period is simply something the scientists who invented the pill designed to mirror the normal menstrual cycle.
The Patch
Like the pill, the patch contains estrogen and progestin that are absorbed through the skin to prevent pregnancy by stopping ovulation from occurring, explains Harrington. Not only does it stop your body from releasing an egg, but the hormones also thicken your cervical mucus, which makes it harder for sperm to get through.
You can wear the beige-colored patch, which is flexible and waterproof, on your upper arm, belly, butt or back. A fresh patch is applied weekly for three weeks, followed by a week off when you’ll get your period.
The Ring
Just like the pill and the patch, the ring, or NuvaRing, is a combined hormonal birth control method—the only difference being that the hormones are slowly absorbed through the mucus membrane inside the vagina. The small ring is about two inches wide and is soft and flexible, slowly releasing estrogen and progestin throughout the month.
The ring, which you insert yourself, should be in place for three weeks, and removed at the end of the third week on the same day of the week and at the same time of day as it was inserted. After a week without the ring inserted, during which time you’ll get your period, a fresh ring is inserted. The ring should be stored at room temperature, but any that you don’t plan on using for four months need to be kept cool (which is why you may have noticed some of your friends stashing their birth control in the fridge).
Progestin-Only Hormonal Birth Control
The Mini Pill
The mini pill, or progestin-only pill, was designed with women who can’t use estrogen in mind. And because it doesn’t contain estrogen, it’s also safe for breastfeeding mothers, shares Harrington. Unlike the combination hormonal methods, the mini pill doesn’t rely on stopping ovulation. Instead, the low dose of progestin works by thickening the mucus in and around the cervix (the lower part of the uterus that connects to the vagina).
“The hypothesis is it blocks ovulation sometimes, but its main mechanism of action is thickening the mucus,” says Harrington. “It’s not a hospitable environment for the sperm to ascend to find the egg.”
OB-GYNs recommend taking any birth control pills at the same time every day, but that tip is crucial when using the progestin-only pill, says Harrington. If you take the pill more than three hours past your usual time or miss a pill, the mucus may already be thin enough for sperm to get through, and so a backup method like condoms are recommended for at least two days. And if you’ve ovulated, there’s a chance you’ll wind up with an unplanned pregnancy, she says.
Unlike the combination pill, you take a hormonal pill every day and you might not get your period at all. Some women do complain about irregular and unpredictable spotting, says Harrington, which is a result of the thinning of your uterine lining that occurs from taking progestin-only birth control.
Injection
The birth control injection, or Depo-Provera, is a progestin-only method that prevents ovulation, providing three months of pregnancy protection per injection, Harrington explains. Since the dose of progestin varies from product to product, so do the effects—which is why the birth control injection stops ovulation and the mini pill might not, she says.
Expect to not have a period—or to have some irregular spotting—if Depo-Provera is your birth control method of choice.
Long-Acting Reversible Contraception
Contraceptive Implant
The1.6-inch progestin-based contraceptive implant, NEXPLANON, is a rod that’s placed in your inner upper arm. Other people can’t see it, but you can feel it under your skin if you touch the area, and it needs to be both inserted and removed by a healthcare provider. It slowly releases progestin and prevents pregnancy by both blocking ovulation and thickening your cervical mucus, shares Harrington.
To insert the implant, your healthcare provider will use an inserter attached to a needle, deploy the device and remove the needle. And while it may seem like it would be uncomfortable to have a small rod in your arm, Harrington says the most uncomfortable part is getting injected with the numbing medication used, which “kind of stings.”
The implant can stay in your arm for three to five years, but can be removed any time before that if you want to become pregnant or feel like you need a method change, she says.
Hormonal IUD
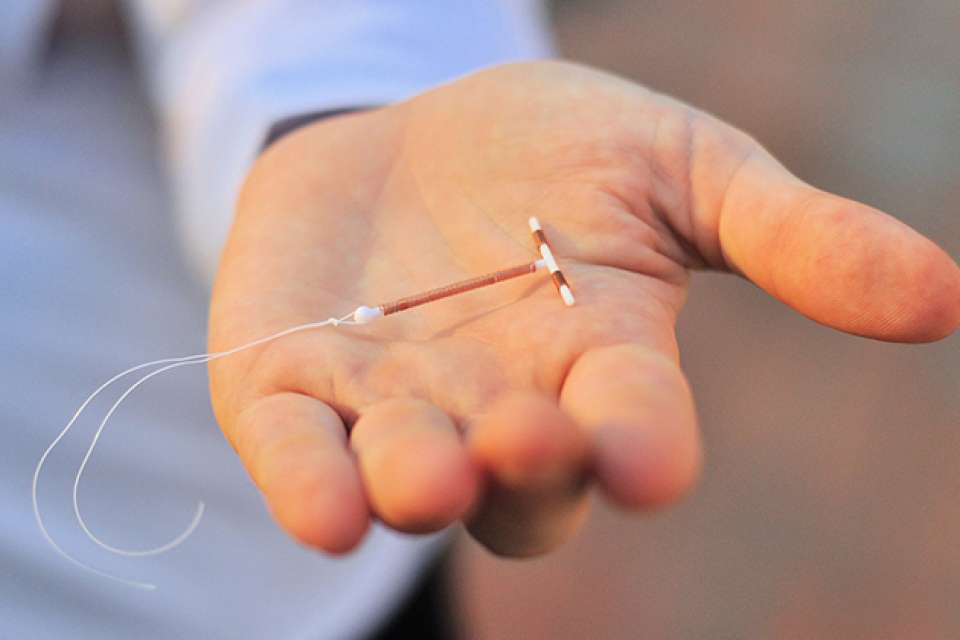
The hormonal intrauterine device (IUD), which is sold under the brand names Mirena, Kyleena, Skyla and Liletta, is a small piece of T-shaped plastic. It’s implanted in the uterus by your healthcare provider to prevent pregnancy for three to six years, but can be removed at any time.
There are a few ways the hormonal IUD, which is a progestin-only method, prevents pregnancy. The main way is by thickening the cervical mucus, explains Harrington. It sometimes stops ovulation, but not reliably, and may affect the way your fallopian tubes move so that it’s harder for an egg to even get anywhere close to the sperm. All of these methods make it really tricky for sperm to get to an egg, she says. “All these different methods combine to make it 99.8 percent effective.”
Copper IUD
ParaGard, the only copper IUD on the market, forgoes hormones in lieu of a tiny piece of copper that’s wrapped around the plastic, and it can prevent pregnancy for up to 12 years. The copper ions create an environment that’s toxic to sperm, explains Harrington. So while sperm might get through the cervix, they don’t stand a fighting chance of reaching an egg. It also causes a reversible process of mild inflammation in the uterus that’s not a good place for an egg to hang out and get fertilized.
The inflammation is limited to the uterus, so it doesn’t cause health problems, and the inflammation doesn’t stick around once the IUD is removed, says Harrington. That means that it won’t affect your fertility later in life.
Since this method is totally non-hormonal, you’ll get a natural menstrual period, but the copper IUD tends to lead to heavier, crampier periods, says Harrington.
Choose What's Best for You
At the end of the day, choosing a birth control method that’s right for you should start with a conversation with your healthcare provider. Together, you can decide which option is best for your health and your lifestyle.

 Healthy ideas for your inbox
Healthy ideas for your inbox





